TreatmentTreatment of MPD is difficult due to the various core characteristics of the disorder. Breaking through the intense secrecy to access the personalities and the traumatic memories is a first step. Then treatment is continually compromised by dissociation, the impaired continuous memory, and switching in response to stress. The individual lacks a stable observing ego, which affects the patient’s ability to report history, to learn from experience, or to have insight. Because the various alters may have different issues, different feelings, and a different sense of commitment to therapy, it is important to get the system to agree to work toward common goals. (Kluft, 1989b) The internal conflicts among alters, the power struggles and the switching will create endless crises. One alter may harm another for sharing information, or another may completely withdraw the patient from therapy. The alters must be worked with to put their narcissistic investments aside, and must begin to empathize, to identify themselves as a whole, and to compromise in order to eventually work cooperatively as one. Braun suggests the therapist must be aware of and address four specific issues: (Braun, 1990)
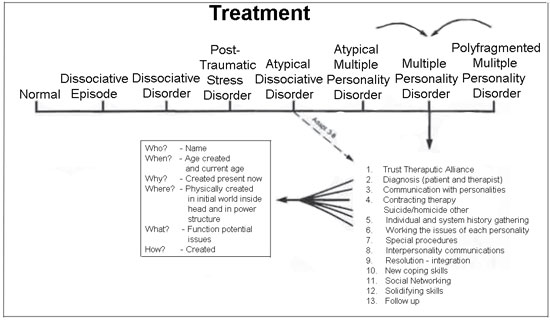
Figure 3. A 13-point approach to treatment of multiple personality disorder. Note. From "The BASK Model of Dissociation" by B. G. Braun, 1988, Dissociation, 1, p. 20. Copyright 1988 by Dissociation. Reprinted by permission. APPROACH TO TREATMENTReferring to figure 3 (Braun, 1990). Braun discusses a 13-Point approach to treatment of MPD. Although the therapeutic issues are shown in a particular order, in therapy they can be worked on back and forth to capitalize on whatever treatment issues is at hand, and to go with the general flow of therapy. Summarized below: TRUST – Enough trust to continue the work of a difficult therapy. Must be reinforced and reestablished throughout the therapeutic process. Must be established with each personality. Rarely complete until the end of therapy. DIAGNOSIS – The diagnosis is difficult to make and difficult to share, It is done in a gentle manner when the patient is comfortable in therapy and the therapist has sufficient data and observations to present in a matter-of-fact way, Reactions of the patient can include relief, recognition, fear, and disbelief. (Steele, 1989) It can feel very frightening to a patient not only because the disorder carries with it certain preconceived notions, but because he secret of childhood abuse, which the whole system has worked so hard to conceal, has finally been exposed. The abused child is terrified of exposure and the alters who have been created to handle that abused child’s life may now act out in any number of ways. The therapeutic team must be aware of this and deal with the behaviors of the various alters as necessary, It is important at this juncture to help the patient feel safe, now that the dreaded secret is out. COMMUNICATION WITH PERSOSNALITIES – Now that the initial trust has been established and the diagnosis shared the therapist will seek to communicate with each personality. The patient may be more comfortable communicating in a less direct way than traditional psychotherapy. Adjuncts such as art therapy or play therapy can be very useful. Hypnosis to draw out reluctant alters is also helpful. CONTRACTING – Contract with the alters to attend treatment and to agree to not harm themselves, other alters, or the body they share. The patient must constantly be evaluated for self-destructive behavior, particularly after a therapy session where a disturbing memory may have been accessed. Contracting, whether verbal or written, should be done as often as needed. This could be anywhere from once a day to every hour. Engage the patient’s cooperation in gauging these feelings. Encourage them to let staff know when they have strong self-harm impulses, and also encourage them to participate in the suicidal precautions by having them report to the nurse at the appropriate time for check-in, rather than the nurse necessarily having to seek them out. This helps the patient to develop a new coping mechanism; recognizing a feeling and, rather than internalizing it, going outside themselves to seek help. INDIVIDUAL AND SYSTEM HISTORY GATHERING – Much of the patient’s history will be gathered indirectly at first. The therapist will gain certain information during a session; however other information will leak out gradually during the course of a day, in occupational therapy, in a group session, over dinner, in interactions with various staff members. It is important to be aware of and document all pertinent information as it is disclosed. Note, in particular, information about the alters, e.g. origin, function, problems, relation to the other alters. SPECIAL PROCEDURES – Can be used as an adjunct to psychotherapy.
INTERPERSONALITY COMMUNICATION – This is a step toward co-consciousness and integration. During the therapeutic activities mentioned above the presenting personality can be encouraged to share information with the others. Hypnosis is helpful with the step. RESOLUTION AND INTEGRATION – Personalities blend rather than continue power struggles. Integration is generally followed by a period of physiologic adjustment that can last days Staff should be aware of the patient’s heightened sensitivity to stimuli, such as light and sound, and uncoordinated body movements. Attention should be given at this time to the types of physical activities the patient participates in, as well as sleep or eating disturbances. NEW COPING SKILLS – Patients learn and develop new intrapsychic defenses and coping mechanisms. Nursing staff can help patients to practice and solidify new skills, particularly as issues arise within the milieu of the hospital. Staff can validate the patient’s feelings or responses to a situation and point out gains the patient demonstrates in ability to deal with a situation in a healthy adult manner. SPECIAL NETWORKING – Find, support/after care groups within the community. SOLIDIFYING SKILLS – As treatment progresses, reinforce positive gains and development of non-dissociative coping strategies. FOLLOW-UP – It is important for the patient to continue therapy even after integration has been achieved to prevent relapse. Patients who abandon therapy after integration generally relapse within two to twenty-four months. This goal of treatment is integration of the different personalities into a unified whole. However, sometimes all that can be achieved is to eliminate the conflict between personalities so that they can work collaboratively, rather than independently or antagonistically. This is a frightening process for an MPD patient. The different personalities have protected the individual from uncovering the painful memories. Giving them up means having to face the hideous trauma alone. Since these personalities have actually kept the person alive, losing them can make the individual feel quite vulnerable. Also, integration may feel like homicide to the personalities, who each consider themselves separate and vital beings. They will resist treatment vehemently. A therapist can reassure the patient that the intention is not to kill off the personalities. The emphasis is that each of the personalities is important and all ideas will be incorporated and addressed. The therapist will teach them how to be angry and how to have power in an appropriate manner so that the individual need not feel victimized again. The personalities are encouraged to develop compassion for one another, rather than antagonism. The objective of treatment is to increase the individual’s ability to function in the world and it can be done with the cooperation and commitment of all the personalities. Integration refers to the mutual acceptance, empathy, and identification of all the different personalities. It is a process rather than a specific event. (Steele, 1989) Barriers are broken down and the personalities are able to come together. This does not mean that one alter becomes dominant or that a new healthy alter is created, or that suppression of alters occurs, giving the appearance of resolution. (Kluft, e) Integration is described as three stable months of:
The recommended treatment of choice is psychoanalytic psychotherapy. Treatment modalities which are not seen as effective are analysis, behavioral approaches, or purely interpretive psychoanalytic therapy. (Kluft, e) Two sessions per week at a pace that allows the patient respite from continuous exposure to the traumatic material is suggested. Because the emotional needs of the MPD patient can be endless and exhausting, the therapist must set firm, but non-punitive and non-rejecting limits. Once the amnesia is broken through, the patient will be in a state of chronic crisis for a long time. (Kluft, e) Though the feelings and functions of each personality are respected, this does not mean the professional condones irresponsible or socially inappropriate behavior. It is always important to protect the patient from dangerous behavior. An important part of therapy is for the patient to learn how to live and function in society. The patient often mistrusts the therapist’s motives in therapy. Trust is important in any therapeutic alliance and even more so with the MPD patient who learns to distrust at an early age. The patient will constantly test the clinical team’s commitment and integrity, and the team must make all attempts to respond with consistency and professionalism. Family therapy with the patient’s family of origin is generally not recommended in an adult MPD patient. The trauma usually comes from this family, and encountering them in therapy causes retraumatization of the patient. However, if the patient is a child, family intervention would be advisable. Therapy involving the patient’s spouse and children is important in helping these significant others deal with the patient’s unusual behavior, to help them gain an understanding of the disorder, and to offer them support. HOSPITALIZATIONPatients with MPD should be treated on an outpatient basis as much as possible. (Kluft, 1991b) There is concern that hospital settings cause the patient to regress, as well as disrupting the continuity of ongoing therapy with the outpatient therapist. An important aspect of outpatient therapy is to pace the treatment in such a way as to minimize the risk of the patient becoming overwhelmed, thus requiring hospitalization due to acts of self-harm. However, despite the most careful outpatient treatment, MPD patients do often require hospitalization. They are prone to self-destructive impulses, thus hospitalization of the MPD patient is generally of a protective nature. Often it is helpful to hospitalize the patient in order to better access traumatic memories or to call forth reluctant alters. Because these patients may fear a loss of control if they were to delve too deeply into childhood memories, the hospital can provide a sense of safety and support in order to more freely let down defenses. Length of hospital stay varies with the circumstances of the patient. It could be a few days to weeks for the patient in immediate crisis or an abrupt dysfunctional episode. This often happens after obtaining a difficult memory or a stressful contemporary event, particularly one involving a perceived rejection. Hospitalization might also be for several months for a patient Whose alters are in chronic conflict, are continually sending threatening messages to the system with every therapeutic step, or who are so unstable and unpredictable in behavior that in order to progress forward in therapy they require the protective and supportive confines of the hospital. Group therapy, particularly a heterogeneous group, for the unintegrated MPD patient is generally contraindicated. Because of their high level of suggestibility, MPD patients are very sensitive to the issues of others. They can become quite overwhelmed, producing anxiety and switching which is disruptive to the group process. The group leader must then divert attention from the group to deal with the dissociative behavior, thus causing the other patients to feel the MPD patient monopolizes staff time and receives special attention. The other members of the group can be left with guilt feelings of having caused the crisis in the PD patient. Also, in a heterogeneous group setting, the MPD patient’s material can sound so fantastic that it is disbelieved and the patient is accused of lying or attention seeking. This will make the MPD patient feel unsafe and abused, thus perpetuating the abusive history. Even in a group entirely composed of MPD patients, if allowed to spontaneously share traumatic childhood material, patients will accomplish little more than re-traumatize themselves through the hearing of others’ material. Because MMPD patients in the initial phase of treatment are too disorganized and fragile to participate in interactive group therapy, task-oriented groups are a better option. These include such groups as occupational therapy, music therapy, movement therapy and art therapy. A specific non-emotional activity, such as drawing a tree or making a coffee mug can help the patient to focus and get relief from the constant emotional charge and switching of personalities. Also, the projects created by alters can be used in psychotherapy as a means of helping the host to acknowledge the existence of alter personalities and the experiences that created them. The treatment of MPD may seem somewhat paradoxical. In achieving integration the individual must first separate out all the alters to be dealt with individually in therapy,. The therapist must respect each alter’s individuality and uniqueness, and deal with the memories and issues of each alter before they can be encouraged to cooperate towards the treatment goal of integration. In order to achieve integration the alters must recognize each other, become mutually sympathetic and then empathic, and finally to work together and merge, thus giving up their narcissistic commitment to individual identities. (Dawson, 1990) Hypnotherapy can be a useful adjunct to psychotherapy. MPD can be seen as a chronic misuse of autohypnosis, wherein altered states of consciousness are created to encode different material. Thus, through hypnosis the therapist can better access alters, particularly those who are reluctant to present themselves in therapy. Work done with one alter does not necessarily impact others, so each alter must be drawn out and worked with separately. It is also a good method for working through the amnestic barrier that prevents the host or presenting personality from obtaining childhood memories of the abuse. A specific technique known as abreactive therapy employs hypnosis to help dissociative patients remember the trauma. While in a hypnotic trance patients are guided back through the memory. All sense of time and space are lost and subjects will actually believe that they have gone back into the abusive experience. They will take on the voice, facial expressions and mannerisms of that age. The body will actually remember how it felt and will react as if the abuse is actually occurring. The patient will feel the intense emotions surrounding the trauma rather than dissociating from the feelings. It is the therapist’s responsibility to help the patient feel safe and reassured that further harm cannot occur; that the experience happened in the past and is not happening now. The therapist acknowledges to the patient that the trauma was survived by the child and that the memory can now be survived by the adult. The patient receives validation and acceptance of the experience and the feelings surrounding it, rather than being punished for them as during the original abuse. The patient then processes the experience and feelings differently than when it originally occurred. This work is then communicated to other alters. The treatment team can then help the patient to develop a new blame-free perspective of his or her part in the childhood abuse experience. By working though the traumatic events in a new adult way, rather than the abused child’s fragmented way, the patient makes steps toward integration. Amobarbital (amytal) interviews, sometimes in conjunction with videotaping and playing back to the patient, can be helpful in treatment. Amytal is a sedative hypnotic which helps the patient to relax and better access memories and/or alter personalities. The therapist must be judicious in this type of treatment, however. Although helpful to some patients, it is shocking and overwhelming to others. Patients are able to see for themselves the presentation of various alters. Timing is essential. The clinician must know when the patient is ready for this kind of aggressive treatment. Mapping is another tool used in therapy that helps both the patient and therapist gain clarity about the personality system. It is a diagram that the patient makes of the system by using lines, circles, boxes or any other method of explaining who the different alters are, how and when they came into existence, and what their purpose is. This helps the therapist to understand how the alters interact with each other, and to anticipate potential conflicts during therapy. DISCHARGE CRITERIA In order to be discharged the goals of admission should have been achieved. This generally means the patient has regained control over behaviors, feelings, and impulses or that uncooperative alters have come to an agreement about the therapeutic process. The patient must be able to contract for safety, and demonstrate a sufficient support system for after-care. Continued outpatient work with a therapist is imperative to prevent relapse, and to continue the gains established in the hospital. MEDICATION Though there is no medication which treats the core psychopathology of MPD (e.g. those symptoms having to do with the actions and interactions of alter personalities), most patients have various other co-existing symptoms and conditions which must be addressed if treatment is to be successful. The manifestations of depression, anxiety, panic attacks, phobias, and transient psychoses can interfere with the progress of therapy and can respond positively with medication. The following are medications commonly used with MPD patients: (Kluft, 1991b)
Loewenstein (1991) recommends the following guidelines for the pharmacotherapy of MPD: Rule 1: Use of medications for MPD patients must be understood in the context of the total treatment of MPD. He suggests performing a thorough medication history of the patient with regards to adherence to therapeutic regimes and liability to self-destructive acts. The clinician must determine liability to self-destructive acts. The clinician must determine that the potential benefits of medication outweigh the potential risks. He recommends finding nonpharmacologic interventions for symptoms. For example, if anxiety is the result of conflict among alters, then psychotherapeutic methods should be the primary focus. The entire system must e enlisted in the cooperation with a pharmacologic regime. If one or more alters is absolutely opposed to medication, then this treatment must be withheld until agreement is obtained. The clinician must then work with the opposing alters to establish the reasons for non-compliance, which may be grounded in the childhood trauma. Many MPD patients report the use of drugs during abuse to assure the victim’s compliance. Certain alters ay have valid fears and resistance to the use of drugs in treatment and these issues can be worked out in psychotherapy and/or hypnotherapy. The system needs to agree to take the medication as prescribed, to use it for one body only, to not use it in a self-destructive manner, and to monitor the effects of the medications. To highlight the difficulties of working with the system to cooperate with a medication regime, Loewenstein gives the example of a patient given imipramine for major depressive disorder witnessed in the host personality. The host soon reported feeling improved with no negative side effects from the medication. Within the same session several other alters came forward with different reports of either no benefit from the medication, or terrible side effects, and finally an adolescent alter who admitted to not taking the medication at all, but that she was stashing the pills away to use in a suicide attempt. It was then established that the patient had, in fact, not taken a single dose of the medication. Rule 2: Most problems in the treatment of MPD are not solvable with medications. During the course of treatment for MPD a myriad of problems, crises and symptoms will arise. Loewenstein maintains that these are not caused by disorders or processes which are responsive to medication. Instead, they are caused by conflicts among the alters, a hidden traumatic memory, a current life problem, or passive-influence. He maintains that these are treatable through psychotherapeutic and/or hypnotherapeutic measures, rather than medication, He suggests the clinician begin by doing a thorough system search for the source of the symptom, and to assess to what extent it affects other alters. Rule 3: (A) One must attempt to treat symptoms in MPD that are valid psychopharmacologic targets. (B) Insofar as possible, one must attempt to target symptoms that are present across the “whole” human being, not those localized in separate alters.
Studies have shown the use of propranolo or clonidine to effectively treat the symptoms of hyper-arousal seen in PTSD. (Loewenstein, 1991) Benzodiazepines are often the safest medications to give MPD patients. Clonazepam has also been found helpful in the treatment of PTSD symptoms. Barbiturates and other nonbenzodiazepine sedative-hypnotic medications should be avoided due to their lethality and the high suicide risk of MPD patients.
In general, psychopharmacologic treatment of MPD patients is still experimental. Psychotherapy and/or hypnotherapy are the treatments of choice. The clinician must search the MPD system of the patient to determine the source of symptoms, and then treat them accordingly, rather than routinely giving a medication that may have some immediate benefit without long term results. Next Prognosis |